Types of Screening
- Details
- Last Updated: Thursday, 29 October 2015 17:54
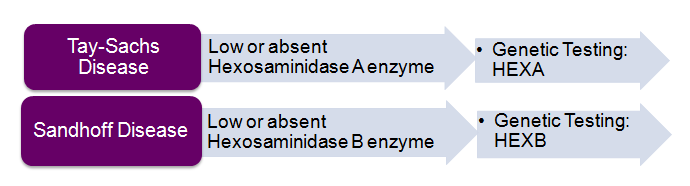
There are two main types of carrier screening tests: Molecular (analyzing the DNA-genetic code) and biochemical (measuring enzyme activity). Carrier screening for Tay-Sachs disease and Sandhoff disease involves a combination of both genetic and enzyme screening for the most sensitive results.
Biochemical / Enzyme Screening:
Enzyme screening is performed using an assay which detects the level of specific enzymes in the blood or a tissue sample. Enzyme assays can be done using serum or leukocytes isolated from blood. For Tay-Sachs disease, screening using serum is the standard of care, but leukocyte screening is recommended when the person being screened is pregnant, on birth control pills, or taking any medications that affect hormones.
The following diseases utilize enzyme screening as the gold standard for carrier screening. Molecular genetic screening should also be performed, as some carriers can be missed via enzyme screening.
Molecular /Genetic Screening:
There are two types of molecular screening:
Most molecular screening only looks for several DNA mutations (changes in genetic code) that lead to decreased production of enzyme. This type of screening often focuses on the mutations seen in one ethnic group and misses those seen in people of other backgrounds. For instance, for Tay-Sachs disease, most molecular screening detects >90% of carriers of Jewish background but only 60% of the mutations found in people of other backgrounds.
The second type of molecular screening is called sequencing. This type of genetic carrier screening is accomplished by reading across the DNA code of a specific gene to determine if there are any known mutations (changes in the DNA code). A negative result significantly reduces the chance that you are a carrier, but it does not eliminate the chance, as it is possible that you carry a mutation that has not been discovered yet or that our current technology is unable to detect. It is important to talk with a genetics professional about how your screening results may impact your family’s health.
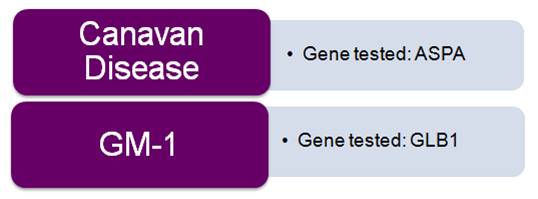
The following allied diseases utilize molecular screening as the gold standard for carrier screening: